Why Does Pain Persist?
Do you have constant aches and pains that persist or keep coming back? Do medications, injections, chiropractic treatments, physiotherapy or massage give you temporary relief but you constantly need these treatments in order to function?
"Perpetuating Factors" may be to blame. These cause you to keep on perceiving the sensation of pain.
How does this work?
Pain is a sensation, so like all other sensations, your perception of it is influenced by many things. Take vision for example. The visual system works as follows:
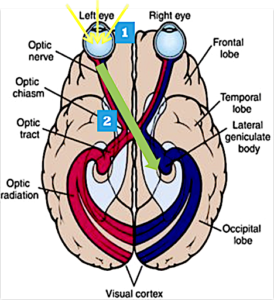
Visual Pathway
- Receptors in your eyes receive light.
- This message is then taken via nerves to the brain.
Areas of the Brain
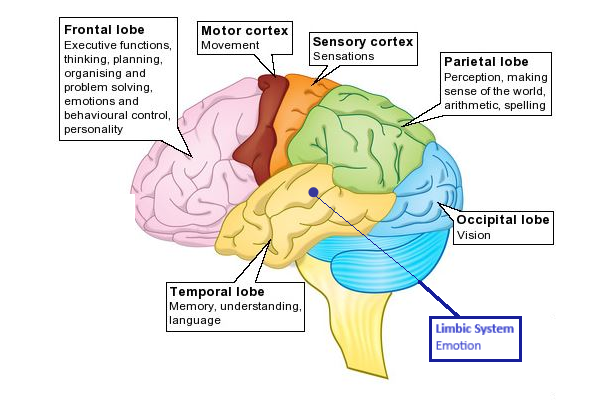
3. Different parts of your brain (eg. the areas that control Attention, Memory, Thoughts, Emotions, etc.) intermingle with the message to provide you with a meaning for what you see and a course of action to take.
4. Certain things (such as a smell, a sound, an image of something) can trigger you to "see" the image of someone or something in your mind even though that object is not present.
So, if a group of people at a party were introduced to a stranger, each person in the group could like, dislike, or be indifferent to the stranger depending on the lighting, the music in the room, each person’s mood, past experiences, alcohol intake, and cultural influences, etc.
How each person acts towards the stranger will determine how the stranger reacts. These actions/reactions will form the basis for an impression of the stranger in each person's mind. If a person has a strong impression of the stranger, then in the future, the stranger's image may appear in the person's mind with certain environmental cues (like a specific song) without the stranger even being present.
Pain works similarly to vision, only instead of detecting light, the pain system detects tactile information such as touch, pressure, heat and cold.
Examples of perpetuating factors of pain are:
- Continuous muscle tension from prolonged postures or repetitive movements that can keep on stimulating the nerves that detect pain in the body.
- Stress and strong negative emotions can intensify your sensation of pain by amplifying the pain signal.
- Negative interactions with others can affect both the physical and psychological components of pain. For instance, if someone is asking (or demanding) you to do a physically demanding task, it can lead to increased muscle tension which can increase pain. Additionally, any anger, guilt, resentment, etc. you have toward the other person are strong negative emotions that would intensify your pain.
So, therapies for pain such as massage, medications, injections, meditation, etc. will only give temporary relief, but the pain will come back unless the Perpetuating Factors are properly addressed.
The reason why the pain system is so important and why it is such a significant source of healthcare expenditure (and human suffering) is that it is your main alarm system. It is meant to irritate you when it detects that something is wrong in your life! Since it is a compass for your well-being, it should not be ignored. In the next few articles, we will discuss strategies to help you with physical, emotional, and interpersonal perpetuating factors.
